Entri yang Diunggulkan
- Get link
- X
- Other Apps
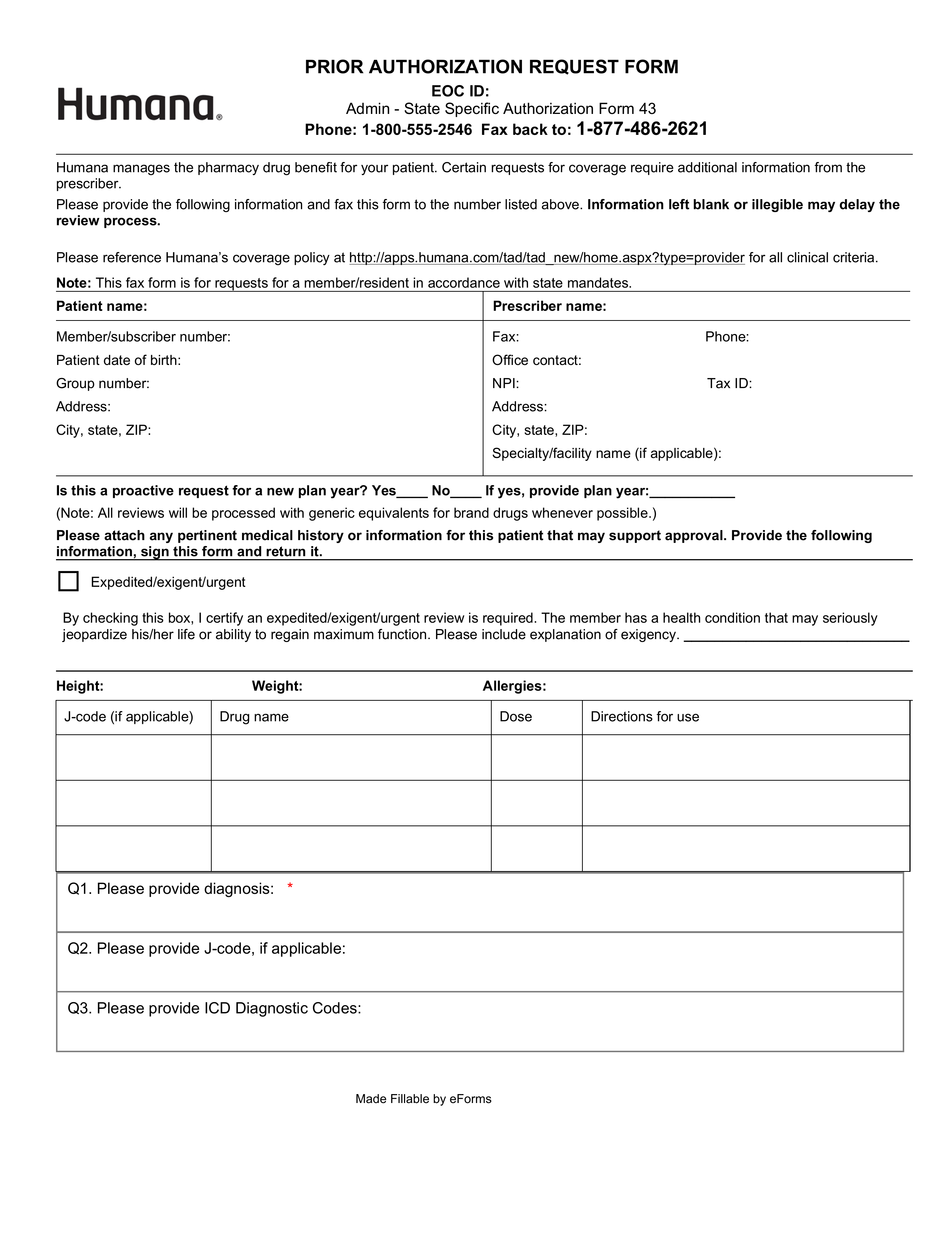
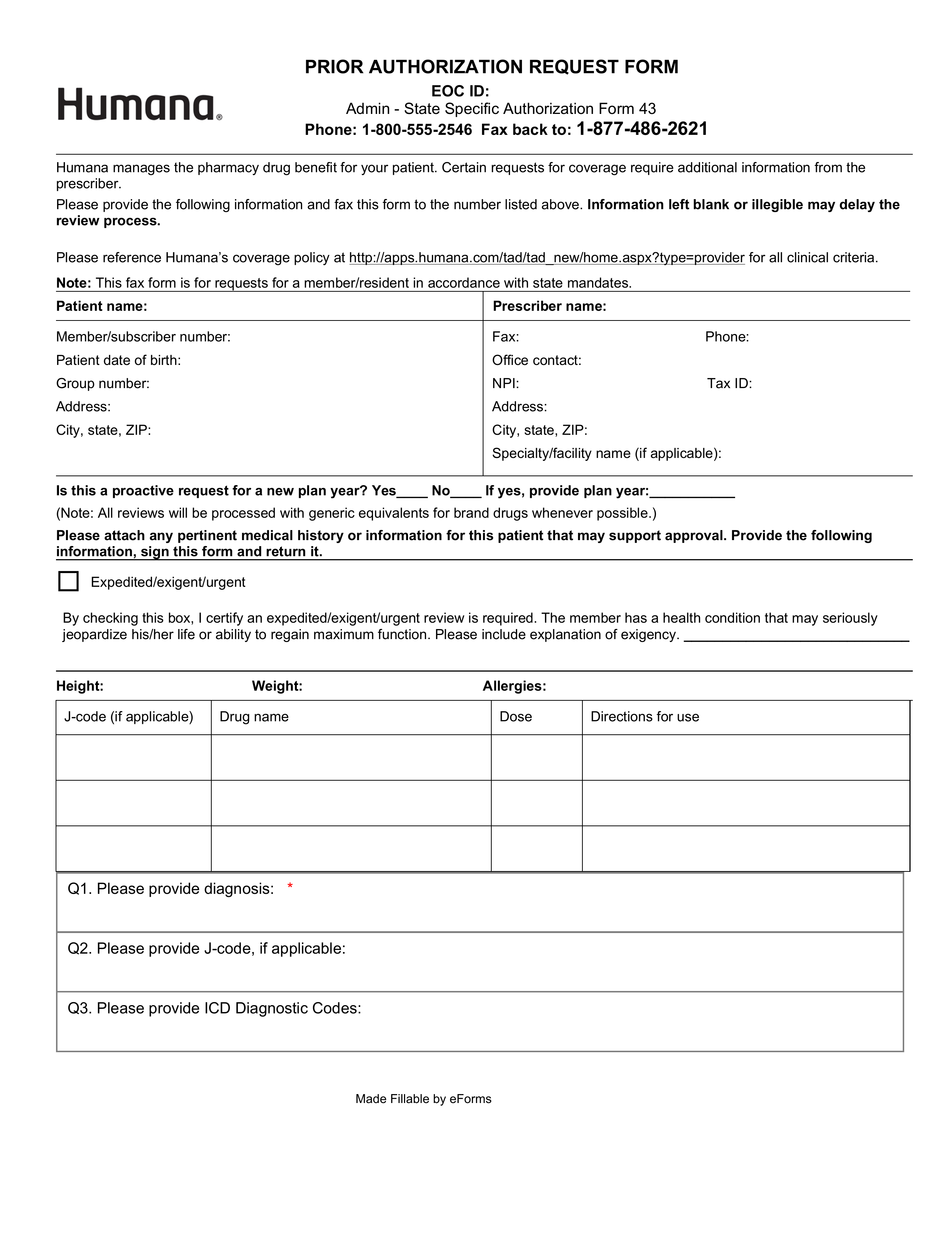
By submitting this form the pharmacist may be able to have the medication covered by Humana. Please complete the form and submit it to Humana by following the instructions on the form.
 Humana Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Humana Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
PRIOR AUTHORIZATION REQUEST FORM EOC ID.
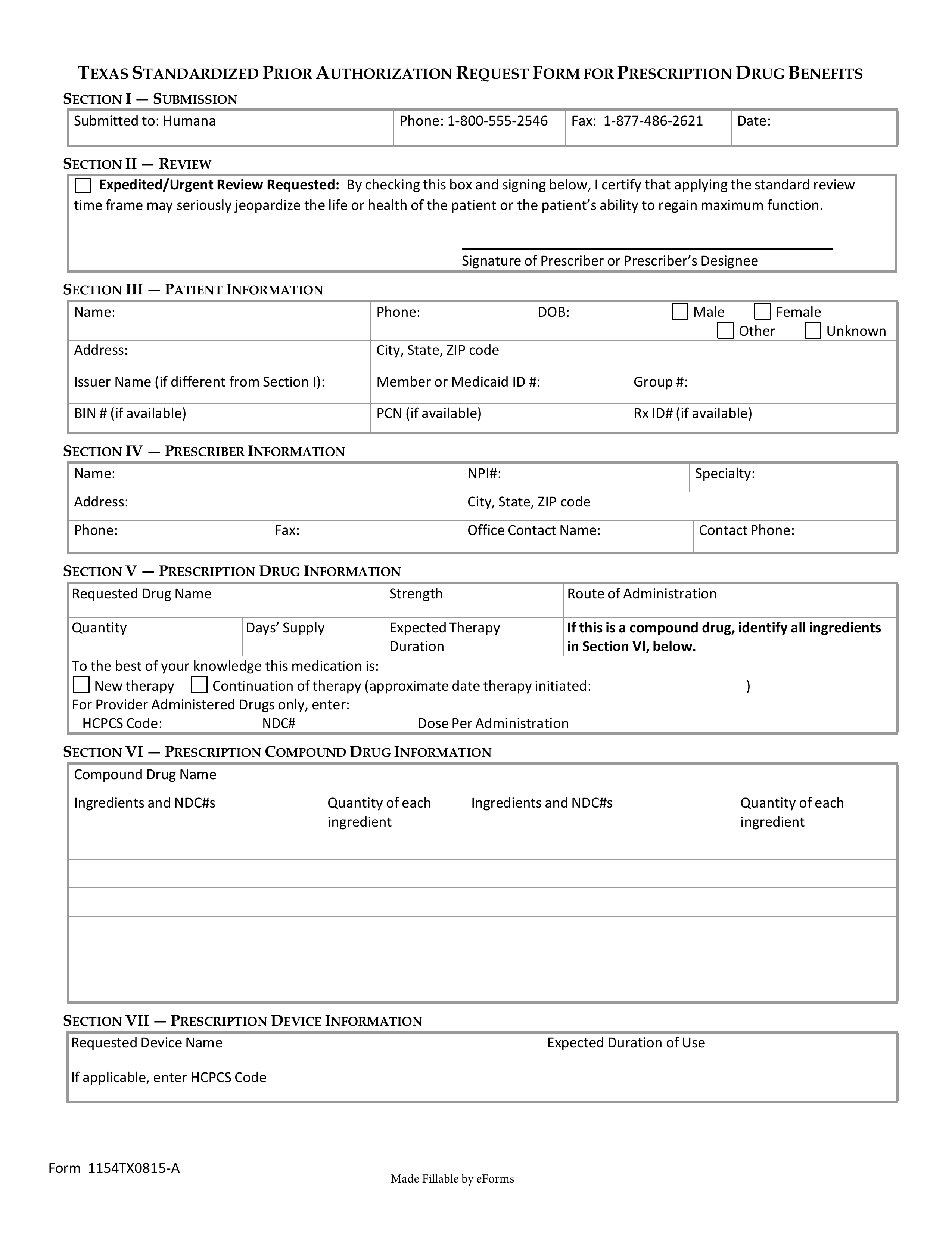
Humana retro authorization. Humana Epic Tackle Electronic Prior Authorizations Member Data The payer and vendor are shifting their focus to implementing an electronic prior authorization. Preauthorization is required for Humana MA HMO and notification is requested not required for Humana MA PPO and PFFS for the following drugs when delivered in the physicians office clinic outpatient or home setting. For certain medical procedures services or medications your doctor or hospital needs advanced approval before your plan covers any of the costs.
We require a signed clinical record submitted with your claim to perform the retro-review. Humana has enhanced its approval process on the Availity web portal with a new preauthorization automation feature. This form does not guarantee payment by Humana Inc.
LC8886KY1120-A HUMP08886 KYHKNQFEN Please note that in addition to the items identified here all DME items costing more than 750 will be subject to retro-review. In addition to commercial issuers the following public issuers must accept the form. On written request Humana CareSource only allow s for a retrospective authorization submission after the date of service when a prior authorization is required but not obtained in the following circumstances.
Admin - State Specific Authorization Form 43 Phone. Humana Healthy Horizons is a Medicaid product of Humana Health Plan Inc. Effective Aug1 2019 Humana CareSource updated retroactive prior-authorization time frame requirements.
1-800-555-2546 Fax back to. Contact us with questions about preauthorization or notification and find out if the services you need are covered in your Humana plan. Illinois authorization request form PDF opens new window.
Responsibility for payment is subject to membership eligibility benefit limitations and interpretation of benefits under applicable subrogation and coordination -of-benefits rules. For all other services please reference the inpatient and outpatient requests to complete your request online or call 1. Vi på Humana har i över tio år hjälpt personer med funktionsnedsättningar att söka personlig assistans och hjälper dig gärna kostnadsfritt med din ansökan och förberedelserna inför din assistansbedömning.
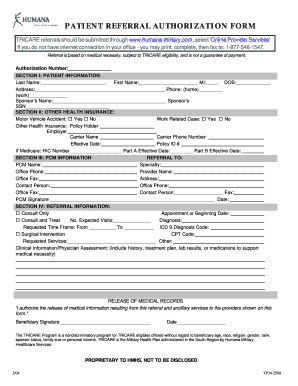
Referralsauthorizations in self-service For Active Duty Service Members ADSM and all other beneficiaries enrolled in a TRICARE Prime plan PCMs must provide a referral for most services they cant provide. Physicians and healthcare practitioners in Illinois should use this form to submit authorization requests for their Humana commercial fully insured covered patients and residents. Humana Prior Rx Authorization Form The Humana Prior Authorization Form is filled out by a pharmacist in order to secure coverage for a patient to acquire a certain medication when they otherwise would be unable to do so.
Det kan också vara skönt att ta hjälp av någon i kontakten med myndigheterna. For TRICARE Select beneficiaries referrals are not required but some services may require prior authorization from Humana Military. Visit the Preauthorization and notifications list online.
Guidelines on retroactive authorizations for services which must be made within 14 calendar days of service extenuating circumstances for those made after 14 days and reconsiderations of a denial. Enrollment in any Humana plan depends on contract renewal. Medicaid the Medicaid managed.
Humana är ett ledande nordiskt omsorgsföretag som erbjuder tjänster inom individ- och familjeomsorg personlig assistans äldreomsorg och LSS. Beginning September 1 2015 health benefit plan issuers must accept the Texas Standard Prior Authorization Request Form for Health Care Services if the plan requires prior authorization of a health care service. This optional feature can provide immediate determinations for requests that previously may have been pended for review.
Find answers to frequently asked questions and how to receive immediate preauthorization determinations. For information on how to submit a preauthorization for frequently requested servicesprocedures for your patients with Humana commercial or Medicare coverage please use drop down below. Humana is a Medicare Advantage HMO PPO and PFFS organization and a stand-alone prescription drug plan with a Medicare contract.
Patient referral authorization form Providers should submit referrals and authorizations through provider self-service by logging into or registering for an account Humana Military only accepts a faxed form if the provider is unable to submit them electronically.
Https Docushare Web Apps Cf Humana Com Marketing Docushare App File 2066922
Https Www Molinahealthcare Com Providers Ky Medicaid Forms Media Molina Publicwebsite Pdf Providers Ky Medicaid Universalpa Map9 R 508c
Https Lakelandcare Com Sites Lakelandcare Com Files Attachments Humana 202021 20coherenext 20step 20by 20step 20training Pptx 20 281 29 20 281 29 20 282 29 20 28002 29 Pdf
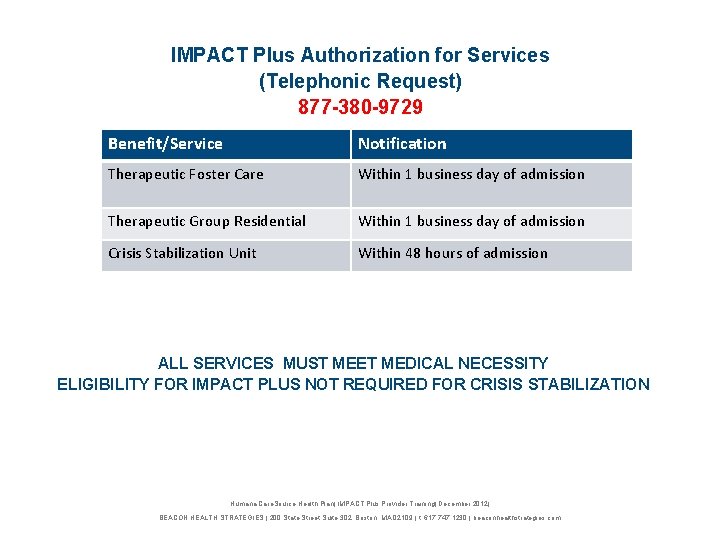 Humana Care Source Impact Plus Provider Training About
Humana Care Source Impact Plus Provider Training About
 Humana Teams With Cohere Health To Streamline Prior Authorization For Musculoskeletal Conditions In 12 States Fiercehealthcare
Humana Teams With Cohere Health To Streamline Prior Authorization For Musculoskeletal Conditions In 12 States Fiercehealthcare
Https Www Caresource Com Documents Ky Hucp0 1151 Retro Authorization Change Notice
 Welcome Firstchoice Medical Group
Welcome Firstchoice Medical Group
 Humana Care Source Impact Plus Provider Training About
Humana Care Source Impact Plus Provider Training About
 Free Humana Prior Rx Authorization Form Pdf Eforms
Free Humana Prior Rx Authorization Form Pdf Eforms
Https Docushare Web Apps Cf Humana Com Marketing Docushare App File 3932669
Https Docushare Web Apps Cf Humana Com Marketing Docushare App File 2502721
 Humana Pcp Referral Form Fill Online Printable Fillable Blank Pdffiller
Humana Pcp Referral Form Fill Online Printable Fillable Blank Pdffiller
Https Www Pswipa Com Wp Content Uploads 2020 04 2020 2021 Provider Manual 2 Pdf
 Free Humana Prior Rx Authorization Form Pdf Eforms
Free Humana Prior Rx Authorization Form Pdf Eforms
Comments
Post a Comment